Making Sense of Diabetes Technology
There is a lot of information showing that people who use diabetes technology have:
- Better blood glucose levels (HbA1c) than those who don’t use diabetes technology.
- Better blood glucose levels (due to using diabetes tech) will enable a child or young person to lead a healthier life with fewer diabetes problems including heart, kidney, eye and feet problems.
- A better quality of life because the tech will sound an alarm to tell you when blood glucose levels are going high or low so you can stop it happening.
- A better night’s sleep because many tech devices have alarms that will sound if there is a problem.

Introduction
The use of technology to support the management of diabetes has increased a lot over the past few years. Technology is widely available and is used as standard practice to manage diabetes in children and young people.
This guide is to introduce diabetes technology to those living with diabetes. You will learn about the different types of technology, what they are used for and what benefits they have. Discuss with your healthcare team what type of technology you would like to use to support the management of your child’s diabetes.

Continuous Glucose Monitors
The traditional method used to monitor glucose levels is to use a finger pricking device with a blood glucose meter and a strip.
Even if you are given or choose to use one of the newer types of technology to monitor glucose levels, you will still be given something like this. It is important to have this as a ‘back-up’ in case the technology fails, you are feeling unwell or if you want to do an additional check.

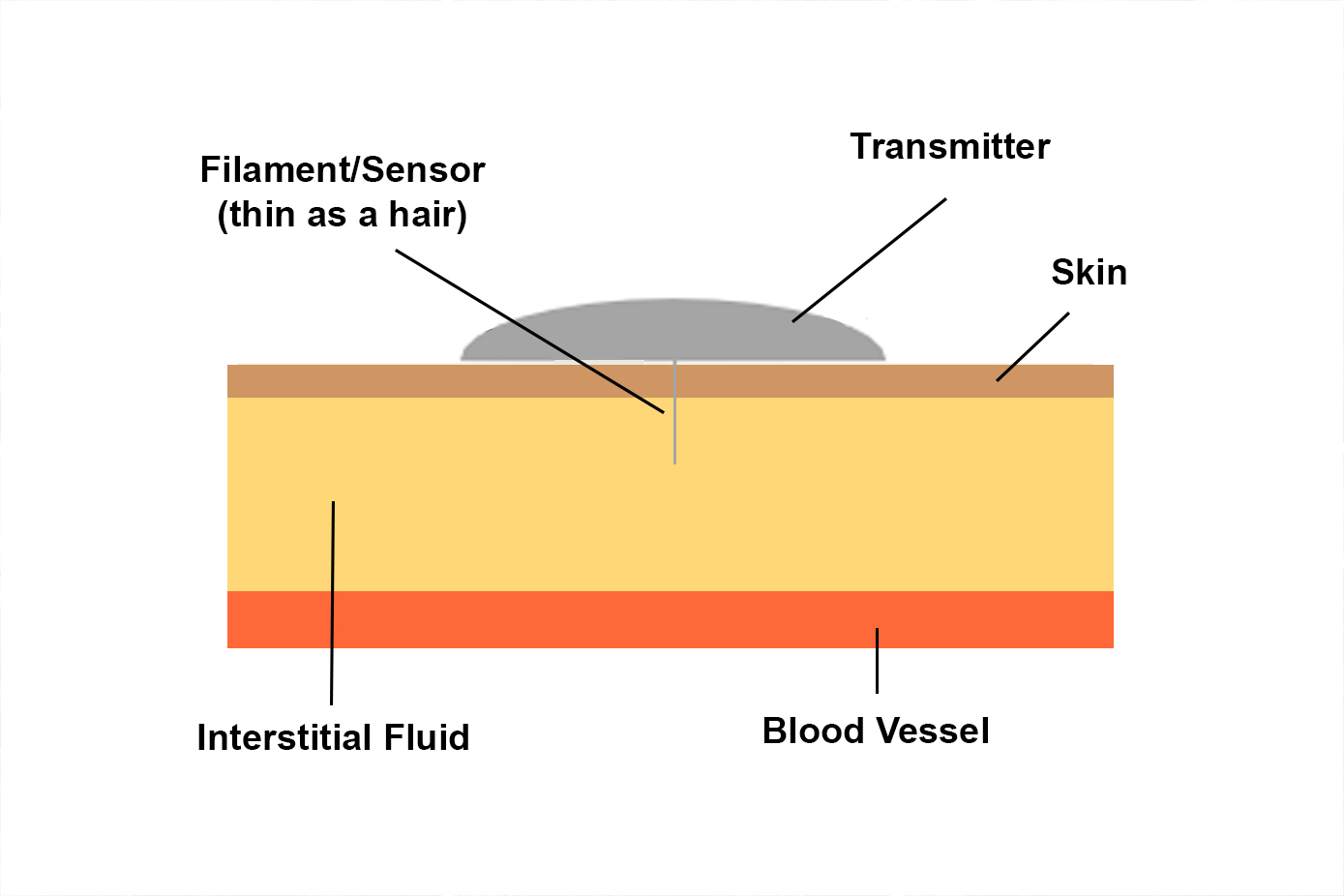
Unlike the finger pricker above, the newer technologies do not use a blood sample to give a glucose level, instead they use a small filament which is as thin as a hair, attached to a sensor which takes the glucose reading from the interstitial fluid just below the skin.
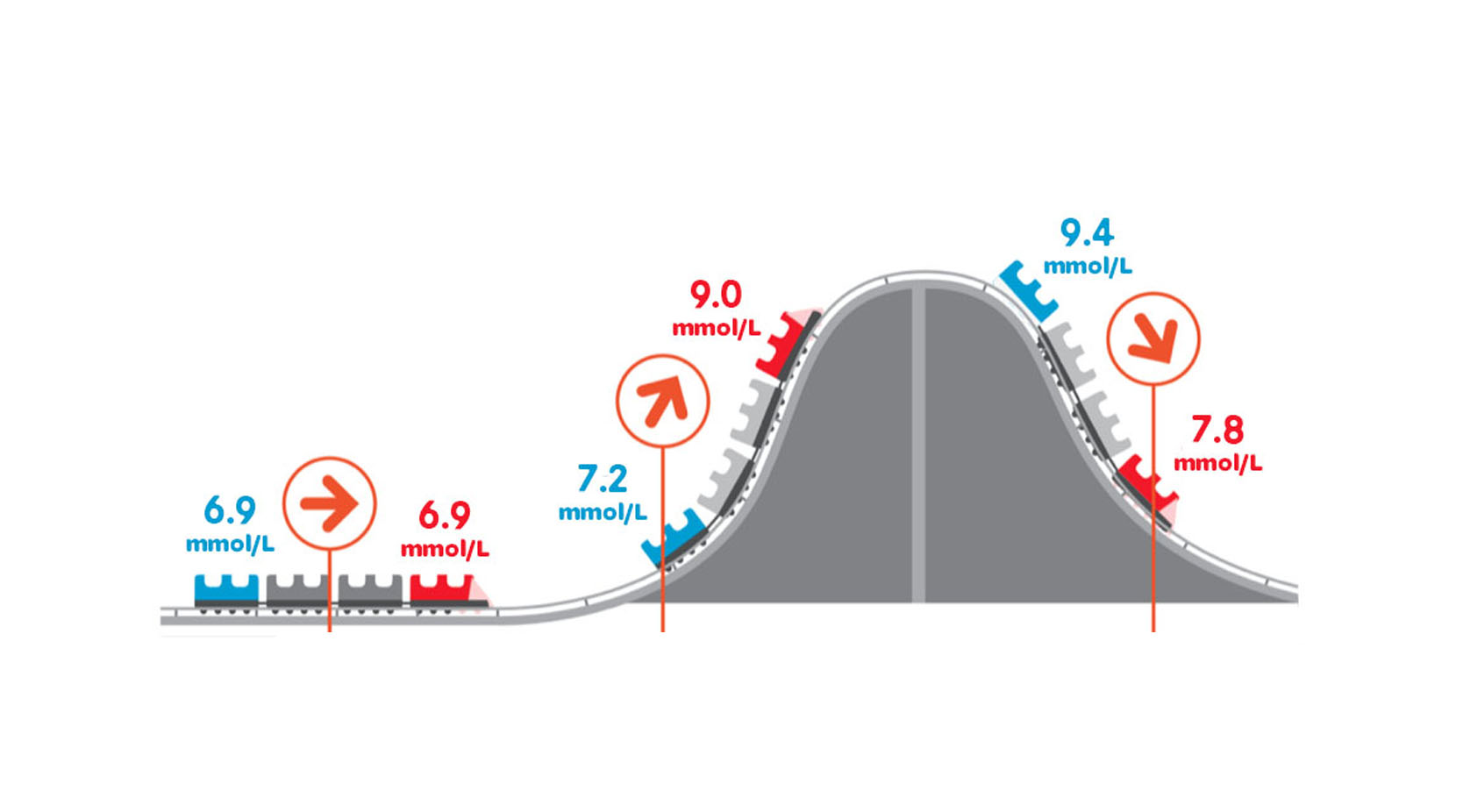
As sensors use interstitial fluid to give glucose readings, the readings are likely to be different from a blood glucose reading. The difference is known as the ‘lag time’ and is usually just under 5 mins.
If your glucose levels are falling rapidly, your blood glucose reading might initially be lower than the sensor reading. If your glucose levels are rising rapidly the blood glucose value might be higher than the sensor reading but then the sensor reading will go higher than your blood glucose value.
- When glucose level is stable, the sensor readings and blood glucose readings are similar.
- When glucose level is trending up, the sensor readings may be lower than blood glucose readings.
- When glucose level is trending down, the sensor readings may be higher than blood glucose readings.
The red train represents the blood glucose reading and the blue train represents the sensor reading.

There are two different types of devices used to monitor glucose, continuous glucose monitoring systems (CGM) and intermittent glucose monitoring systems (iCGM) also known as ‘Flash’.
Continuous Glucose Monitoring Systems - CGMs
A small sensor reads the glucose level in the interstitial fluid and immediately sends the data to a hand-held, pocket-sized machine/reader or a mobile phone which can be viewed at any time. Arrows will also tell you if glucose levels are steady, on the way up or on the way down. There are options to set alarms for high and/or low levels and lots of different ways you can view glucose levels using reports and share them with your healthcare team. Parents and carers can also see the glucose readings and set alarms on their own device.
Continuous glucose monitors are usually made up of three parts:
- A device to insert the sensor.
- The sensor and transmitter – the sensor needs changing every 7-10 days and the life of the transmitter varies with different devices.
- The reader (or phone) - to receive the glucose level


Intermittent Continuous Glucose Monitoring - iCGM or Flash
A small sensor reads the glucose level in the interstitial fluid and when scanned with your reader or phone it will show your current glucose level. Arrows to indicate if your levels are steady, going up, or going down and data from the previous 8 hours is shown. Alarms can be set for high and/or low readings.
iCGM have an insertion device, sensor and transmitter and a reader (or phone) just like CGMs.
The main difference between CGM and iCGM is that when using CGM you can view glucose levels at any time on a reader or phone, without having to do anything. With iCGM a scan of the sensor using a reader or phone is needed to be able to see your levels. You will have to provide a compatible phone device if you wish to use a phone for monitoring glucose levels.
Key Benefits of Continuous and Intermittent Glucose Monitoring Systems
1. Know what is happening with your glucose levels all the time
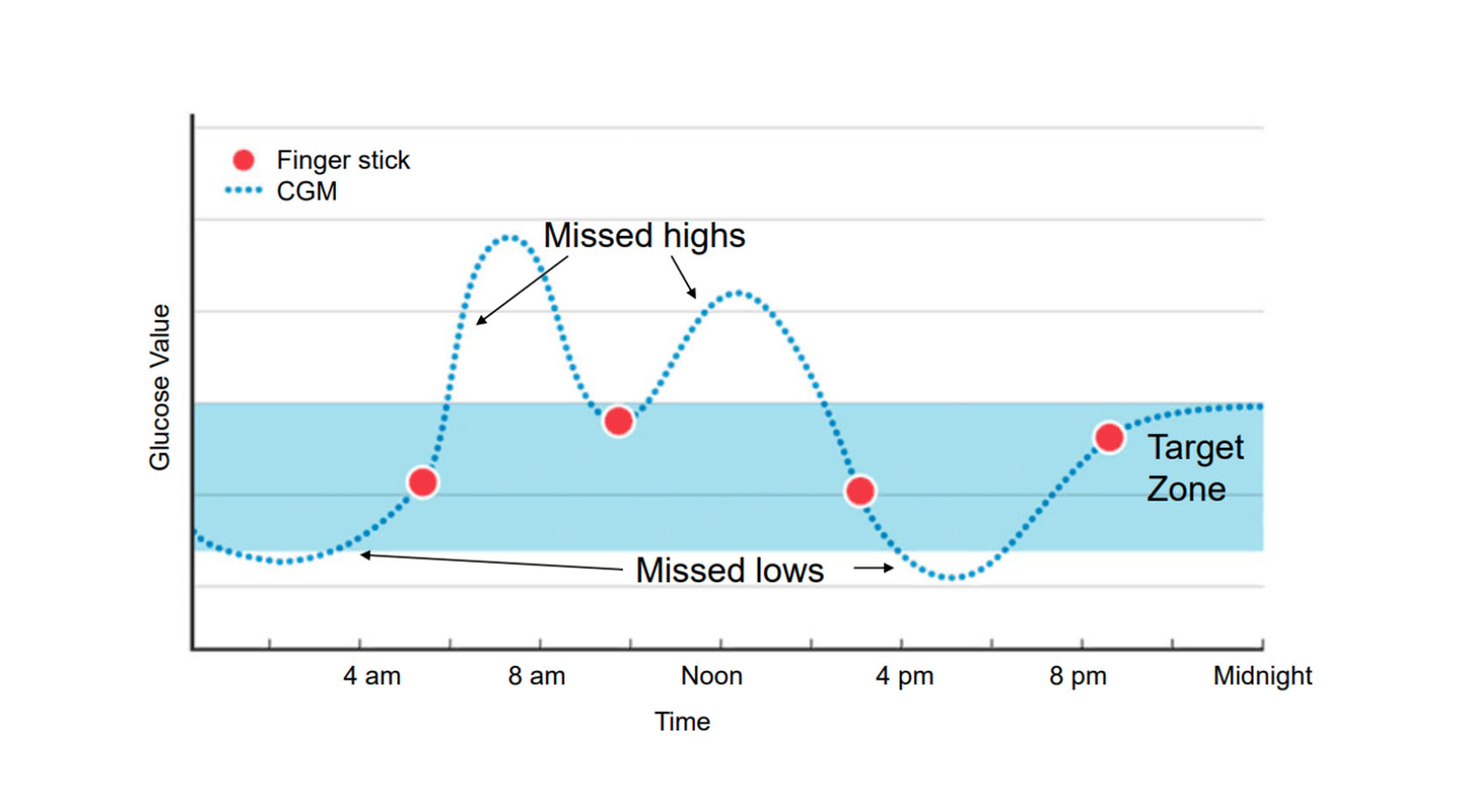
Look at the chart in the image:
- The blue band across the graph shows the target area for glucose levels.
- The red dots show 4 glucose checks using a finger prick.
- The blue dotted line shows what you see using a CGMs or iCGMs.
When you are only using finger pricks to check glucose levels, you only see what is happening in that moment, you can’t see what is going on the rest of the time.
When you use a CGMs or an iCGMs, you can see what is happening all the time and will not miss highs and lows.
2. Peace of mind for parents and carers
The child/young person’s glucose levels and alarms can be shared with parents and carers on their own device (depending on what equipment is used), giving peace of mind that highs and lows will not be missed.
3. Reduced finger pricks
Regular daily finger prick checks are not needed on CGMs and iCGMs, a finger prick check will only need to be done to check that sensor readings match any high or low glucose symptoms. Instead of the inconvenience and pain of regular finger pricks, sensors should only need replacing every 7-14 days.
4. Know where glucose levels are headed
Arrows on the reader/phone will let you know where glucose levels are headed, this will help you to make decisions on insulin adjustments that may be needed.
5. See patterns and trends
You will be able to see how different things like food, activity, the weather, or stress all affect glucose levels and learn how to manage them with adjustments to insulin.
Insulin Pumps
Devices for Delivering Insulin
The traditional method of delivering insulin is to inject a long-acting (basal) and short-acting (bolus) insulin into the layer of fat (sub-cutaneous) below the skin, using a small needle attached to an insulin pen.


Insulin pumps are devices that are designed to deliver insulin without the need to inject. They have been around since 1978 but have developed over the years from very large pieces of equipment to very small devices.
How an Insulin Pump works
1. Basal Insulin (sometimes known as background insulin)
Basal insulin is the insulin that continuously flows throughout the day and is traditionally delivered by injecting a long-acting insulin once or twice a day which works over the course of 12-24 hours.
When you have a pump, instead of using long-acting insulin for the basal, the pump will be programmed to deliver small amounts of fast-acting insulin continuously throughout the day.
The basal insulin can be adjusted to deliver different amounts of insulin for different times of the day and while exercising etc.
Because there is no long-acting insulin working in the background, you should always remain attached to your insulin pump. However, some pumps might need to be disconnected for:
- Showering or bathing
- Swimming
- Sports
If you are disconnected for long periods of time (more than 2 hours), high glucose levels and ketones can develop.
2. Bolus Insulin
Bolus insulin is a dose of fast-acting insulin given with meals, snacks and for glucose corrections when glucose levels are above target range.
Instead of injecting the fast-acting insulin with your injection pen, the pump will calculate the precise dose of insulin needed, based on the grams of carbohydrate eaten and your glucose values. You have to enter the grams of carbohydrate into the pump or handset, and you may also have to enter the glucose value. Once confirmed the pump will then automatically deliver the dose of insulin through the cannula.
Types of Pumps
There are two types of insulin pumps :
- Tubed/tethered pumps.
- Tubeless/patch pumps or pods.

Tubed/Tethered pumps
With a tubed/tethered pump, insulin is delivered from a small pump device that you would have in your pocket, wear on a clip or in a pump pouch. The insulin travels through a thin tube into a cannula which sits just under the skin. The insulin delivery is controlled using the buttons on the small pump device and the cannula must be changed every 2-3 days.
A tubed/tethered pump will consist of three main parts:
- Cannula insertion device.
- Cannula and tube.
- The pump (holds the insulin and controls the insulin delivery).
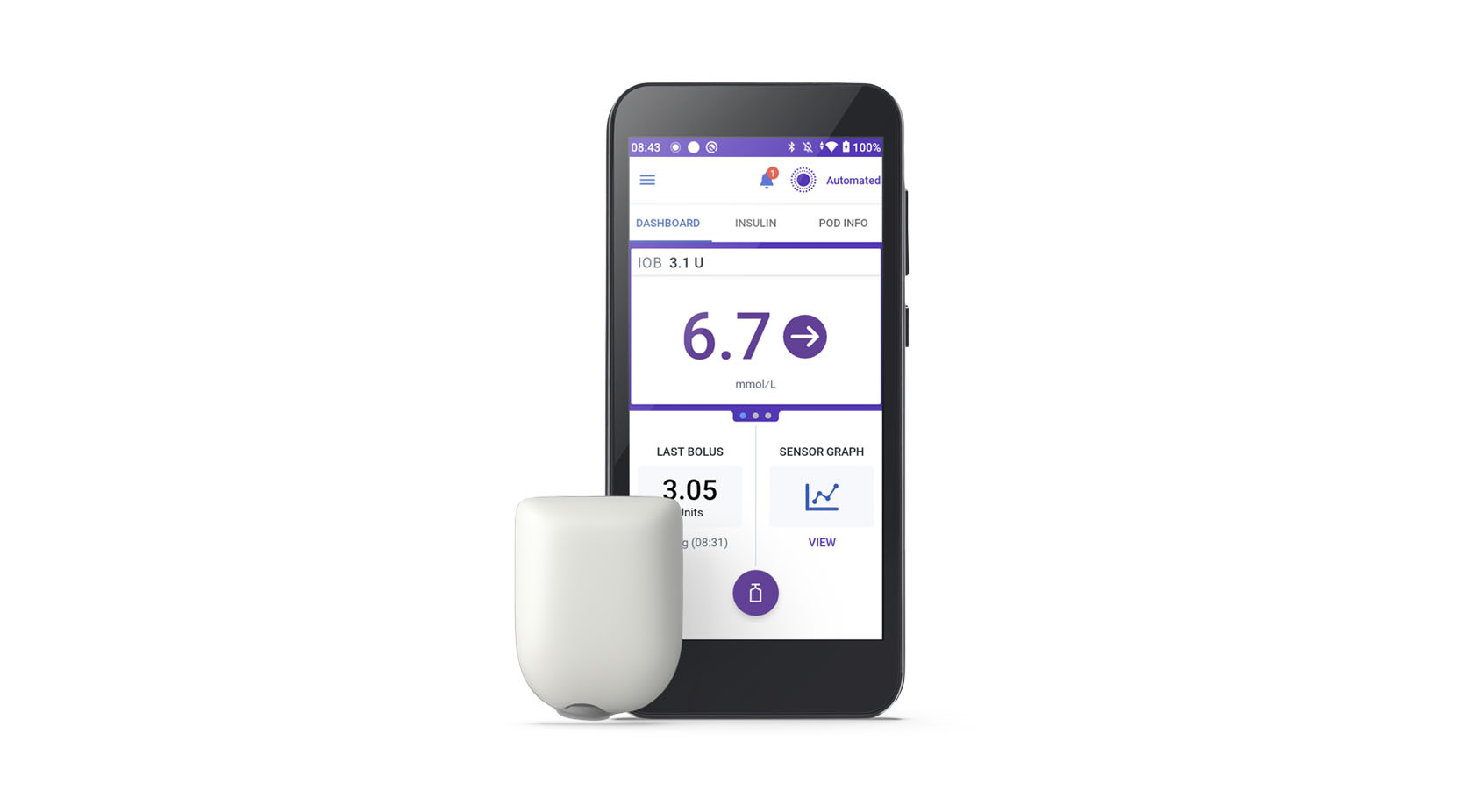
Tubeless/Patch Pumps and Pods
With a tubeless/patch pump or pod, the insulin is held in a small pod which is connected to a cannula and attached to the skin. The insulin delivery is controlled using a handheld device which connects to the pod using Bluetooth. The pod needs to be changed every 2-3 days.
A tubeless/patch pump or pod consists of two main parts:
- The tubeless/patch pump (holds the insulin).
- Handset (controls the insulin delivery).
The tubeless/patch pump can remain in place for sports, swimming, showering, and bathing.
Key Benefits of Insulin Pumps
No injections
You will no longer need to inject your basal insulin once a day and your bolus insulin every time you eat. Instead, you will just need to insert a cannula from your pump approximately every 3 days.
Quality of life
Wearing an insulin pump gives you more flexibility with your daily routine, you can eat whenever you want and easily give insulin.
Flexibility to adjust
The amount of insulin you deliver can be easily adjusted using the pump controls so you can make changes depending on the type of food you are eating and how active you are being. The pump can deliver more precise amounts of insulin than pen injections, including very small doses.
Achieve better control of your diabetes
All of the above benefits mean, if you use your insulin pump well you could get better control of your diabetes so your short-term and long-term health will be improved.
Hybrid Closed Loops
Devices that work together to check glucose levels and deliver insulin (Hybrid Closed Loops)
A hybrid closed loop (HCL) is a system which involves one of the pumps working together with one of the CGMs.
The insulin is delivered using the pump and is controlled by the glucose level information that is sent from the CGM.
An algorithm is like the brain, communicating between the pump and the CGM and is key to making the system work. The algorithm is either held within the pump or on a phone app.
Basal (background) insulin is automatically adjusted to keep your child in range, but carbohydrate grams for food still need to be entered for bolus insulin.

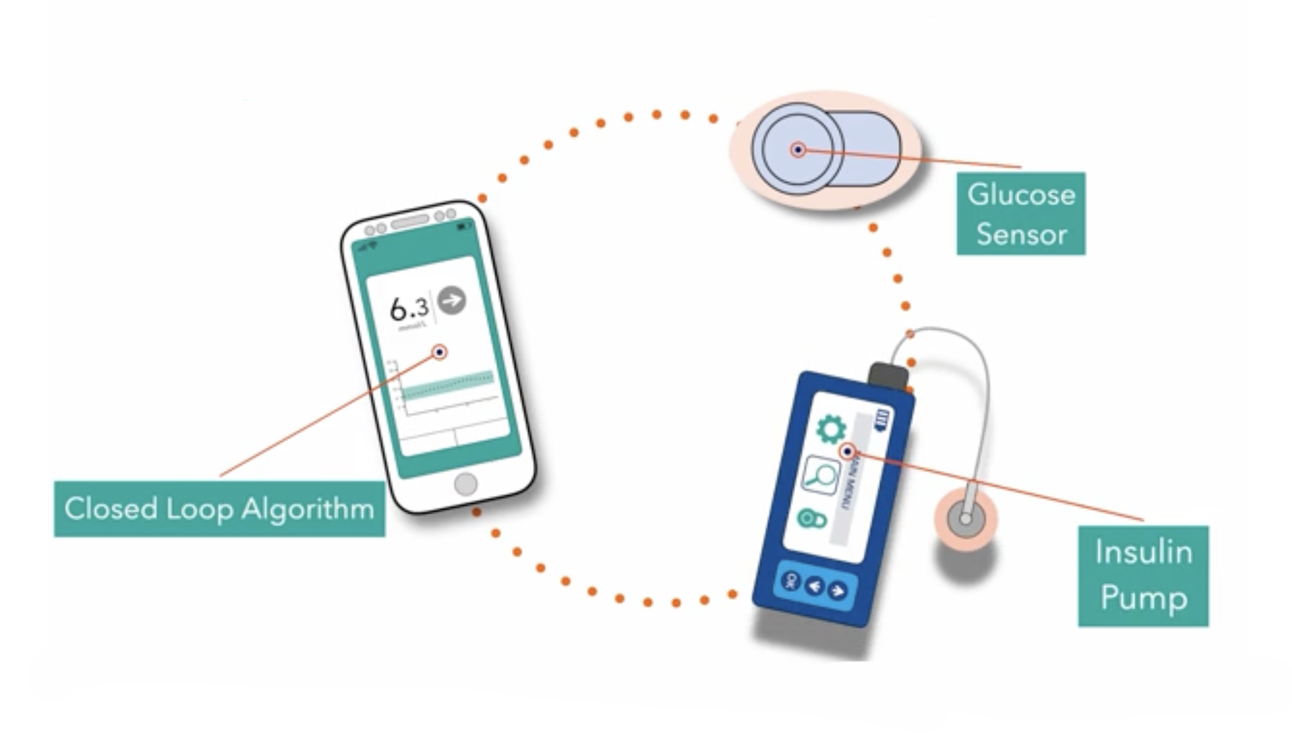
- Check your glucose levels with Continuous or Flash Glucose Monitors.
- If you want, your technology can talk to each other, but for this you will need a Communication tool - Algorithm.
- Deliver your insulin with Insulin Pumps.
- Glucose Monitors and Insulin Pumps can communicate with each other using an Algorithm.
- This creates a hybrid closed loop.
- Glucose Monitors and Insulin Pumps can be used on their own or as part of a complete system (Hybrid Closed Loop).
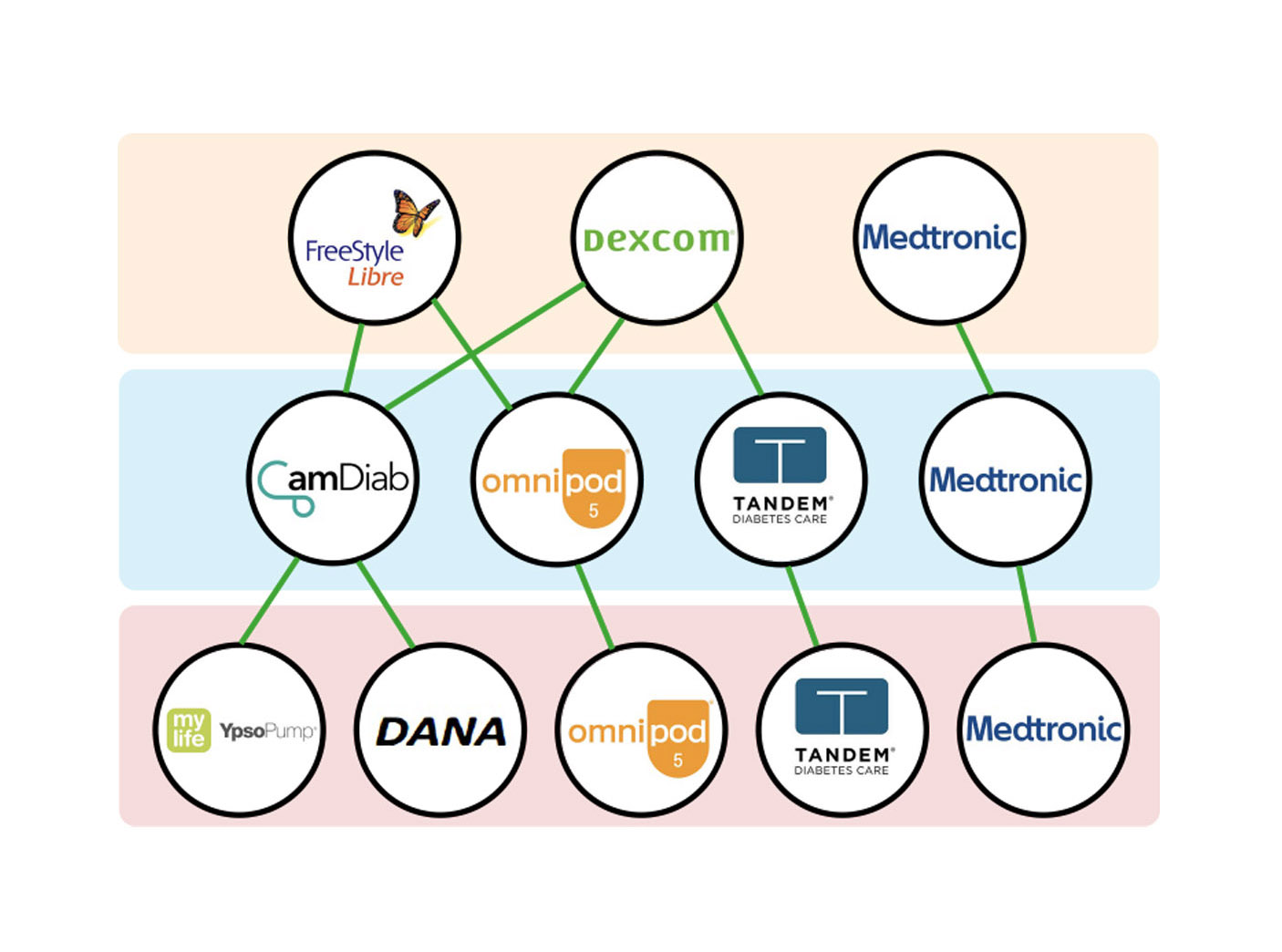
Not all pumps and CGMs work together, this diagram shows the available options.
The Devices
Use these devices to check your glucose levels:
- FreeStyle Libre - compatible with: CamDiab - Omnipod 5.
- Dexcom - compatible with: CamDiab - Omnipod 5 - Tandem.
- Medtronic - compatible with: Medtronic.
Use a communication tool between your glucose monitor and your insulin pump:
- CamDiab - compatible with: YpsoPump - Dana.
- Omnipod 5 - compatible with: Omnipod 5.
- Tandem - compatible with: Tandem.
- Medtronic - compatible with: Medtronic.
Use these devices to deliver your insulin:
- YpsoPump
- Dana
- Omnipod 5
- Tandem
- Medtronic
Key Benefits of Hybrid Closed Loops
As described above, a hybrid closed loop system is the combination of a CGM and an Insulin pump working together. The benefits of using a hybrid closed loop system are therefore a combination of the benefits of using a CGM and an Insulin pump.
Summary of benefits
Less invasive
- You will no longer need to prick your finger to get a glucose reading or give an injection to deliver your insulin.
- Instead, you will wear a sensor that needs changing just a couple of times every month and an insulin pump that needs the cannula changed every few days.
Limited intervention needed from patient
Once you have learned how to use your chosen hybrid-closed loop system all you need to do is:
- Change your sensors and cannulas as required using new skin sites.
- Input your carbohydrate grams before delivering bolus insulin.
- Make sure you regularly review your glucose and insulin data.
Improved outcomes
You will need to trust your chosen hybrid-closed loop system and allow it to work with you to manage your diabetes. Once you can trust it and work with it you will notice...
- Less hypos.
- Less hypers.
- More time in the glucose target range.
- Better HbA1c.
- Less risk of long-term health conditions.
- Improved quality of life.
- Better sleep quality.
Diabetes Technology - Some things to think about
- Your devices are always attached to you (unless required to be removed for showering/sports).
- You can’t just “set it and forget it” – hybrid-closed loops still require you to monitor what is happening with your glucose levels and make any required adjustments to your insulin delivery. You must still enter grams of carbohydrate for all meals and snacks.
- There is a lot to learn in the beginning – it is not an overnight solution! You will need to learn some new skills and take time to understand your chosen device/s.
- You will still occasionally have to check your glucose levels using a finger prick, when sensor reads low or symptoms do not match your reading.
- You will still need to inject your insulin if your insulin pump fails or sometimes when you need to reduce your glucose levels while ill or hyper.
Your healthcare team will offer support and guidance on choosing the right diabetes device/s for you and will ensure you are fully confident in using them. They will monitor and support you throughout your diabetes journey as a child/young adult.