LWD - Chapter I
10 Top Tips for Glucose Management
We encourage regular review of your glucose patterns between clinics and would like to support you to develop skills and confidence to make changes to insulin doses. If you are not sure what to change, or would like some help, please call the diabetes team rather than wait until your next appointment.
Here are our 10 top tips to help you:
1.
Always give insulin before food. 15 minutes before food is best for Novorapid, 5 minutes before food for Fiasp.
2.
Always consider lumpy injection sites (lipos), if glucose levels are variable. To check for these, use 2 fingers to firmly press and move over the skin to feel for lumps. A moisturiser or a shower gel whilst in the bath/shower can help. If you find any, avoid that area for injections and rotate using other sites.
3.
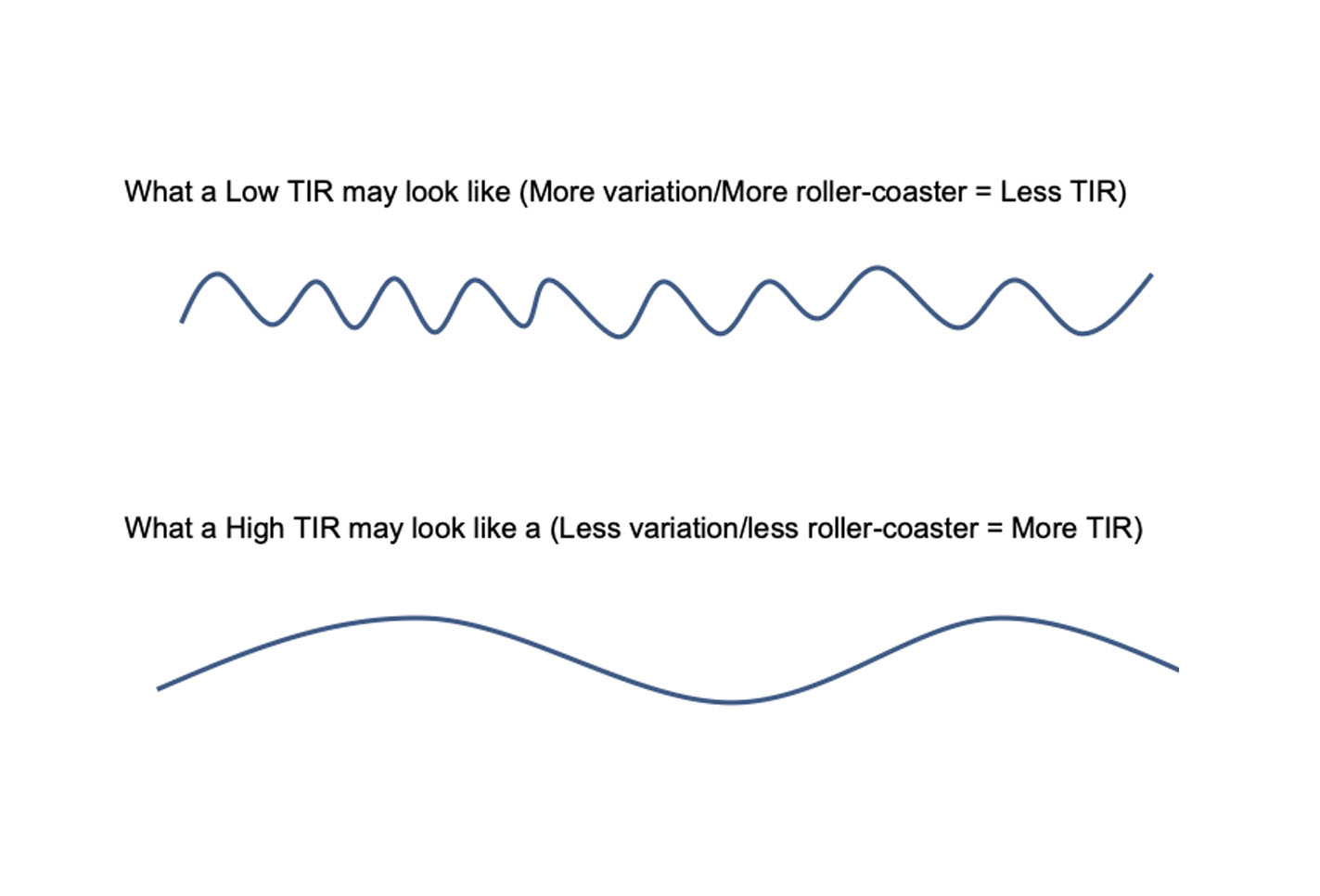
Regularly review your data with your child and problem solve together. You can do this by uploading and reviewing your meter/pump/app or keeping a blood glucose (BG) diary. The ideal glucose level target range is 3.9 – 8 mmol/L. When reviewing your data, review the Time in Range (TIR). For Glooko/Clarity/Medtronic/Libreview the TIR is the length of time spent with glucose values between 3.9 and 10mmol/L. The ideal target is 70% TIR and less than 4% in hypoglycaemia which will help your glucose to remain steady.
4.
Look at the average glucose on the meter/app/download over a 14 day period. An average glucose of less than 8.0mmol/L will help your HbA1c to be close to the 48mmol/mol target. For the average glucose target to be accurate, glucose should be checked, or flash meters should be scanned at least 8 times a day.
5.
Look for frequency of hypos. 2 or 3 mild hypos per week are acceptable, more than this needs insulin reduction. Can your child recognise their hypo? If not, contact your diabetes nurse.
6.
If the glucose levels are above the target range in the mornings (more than 7mmol/L for 3 days or more in the week), check you are in target before bed. If so, increase long-acting insulin. Always optimise basal insulin first before changing mealtime insulin. Please leave 3 days between basal insulin changes to check effect.
7.
How to increase basal insulin (e.g. Levemir/Lantus/Tresiba)
- If your child has less than 10 units of long acting insulin, increase by ½ unit at a time.
- If your child has 10-20 units of long acting insulin, increase by 1 unit at a time.
- If your child has more than 20 units, increase by 2 units.
8.
If the glucose levels are above the target range before bed, change the evening insulin to carbohydrate ratio (ICR) in the mylife bolus calculator, pump or app e.g. if 1 unit of insulin per 10g carbs (1:10), change to 1 unit per 8g carbs (1:8) to strengthen the bolus. This will give you approximately 0.5 to 1 extra unit per meal.
9.
If the glucose levels are above the target range before a particular meal for more than 3 days in a week (over 8mmols), increase the ICR for the meal eaten before the meal with higher levels (e.g. if the glucose level is above the target range at lunchtime, increase the breakfast ICR dose). Check this change has been effective by noticing if there is a rise of no more than 2-3mmols, 2 hours after meals for a few days. Remember, an increase in insulin ratio means a decrease in number e.g. changing from 1:10 to 1:8 will give more insulin.
10.
Always give the correction dose suggested by the bolus calculator at meal times. Consider correction doses at other times if needed, e.g. If glucose levels are more than 8mmol/L at least 3 hours after the last dose of insulin and more than 1 hour till the next predicted time of insulin. If extra corrections are regularly needed, try top tip 8 & 9 or contact your diabetes nurse.