LWD - Chapter E
Preparing For Home
E1: Immediate Support
You will have a named nurse allocated to you on discharge who will offer you either a home visit shortly after discharge from hospital or ask you to go to the diabetes centre (especially if you’re starting on CGM. IPT or AIDs). The dietitian will also be involved in this visit.
Your team will be in touch regularly as you settle into life with diabetes and your new technology. If you/your child attends school or nursery, a diabetes nurse will go into school shortly after discharge to discuss with staff how to manage diabetes in school. It is helpful for parents and children to attend this first meeting so that a care plan can be discussed and agreed. Parents may need to go into school initially until the designated staff have learnt how to manage all aspects of caring for diabetes within the school environment. School staff will be asked complete an E learning course on DigiBete and attend a school workshop to receive comprehensive education about diabetes management in school, and practise using the equipment.
E2: Disability Living Allowance
All children with diabetes under 16 years old are eligible to apply for Disability Living Allowance (DLA). This is not means tested and does not mean that your child will be registered as disabled. The payment is to help with the extra care and attention that children with diabetes require. It is not usually paid to children over the age of 16, unless there is another medical condition; then you could apply for Personal Independence Payment (PIP).
You may obtain forms from the benefits agency on 0800 121 4600. Alternatively, you can complete the forms online. Your specialist nurse will be able to help you.
If you are applying or at university, you can apply for Disability Student Allowance via your University. This can help to secure you accommodation with en suite and a fridge for your insulin.
E3: Clinic
You will be invited to an outpatient clinic appointment once a month for the first three months following diagnosis with diabetes, then once every three months after that. You will be encouraged to look at your own diabetes data in between clinics and get in touch with your named nurse if you need advice.
At clinic, you will see a Diabetes doctor, nurse and a dietitian who will answer any questions you have, review your diabetes data and give you advice. They will check your height, weight and HbA1c every time you go to clinic and will explain why they monitor these things (and what they mean) in your first appointment.
In one of your first three clinic appointments, you will meet a diabetes clinical psychologists; a diagnosis of diabetes is a big event and it is normal to experience a number of feelings such as sadness, shock, anger and upset. If these feelings continue, and you or your family find it hard to deal with these, the psychologists are there to help.
E4: Ongoing care
Your diabetes team is always there for you – they want you to feel confident to manage your diabetes independently but are always there to offer support, guidance and advice. Appointments can be organised outside of clinic with your nurse, dietitian, psychology, play specialists or the youth work team.
Annual Review
Once a year you will be invited to an “annual review” clinic. This is where they will check your urine to make sure your kidneys are working well, do a blood test from a vein to screen for coeliac and thyroid disease, and cholesterol if over 12 years old. Your team will talk about your feet, your eyes (from the age of 12 you will be invited to a retinal screening appointment every year/every other year) and look at your injection/cannula sites.
Persistently high glucose levels can put certain body parts at risk as they can damage your blood vessels. Aside from trying to maintain your time in range around 70%, other things you can do to help yourself/your child are to look after your feet by wearing slippers or shoes at all times. Don’t ignore ingrown nails, cuts or blisters and tell your team if you have any problems with your feet so they can refer you to a community podiatrist. Other things are; to look after your teeth by brushing twice a day and have regular dentist check ups. Tell your dentist that you have diabetes and if you require any dental surgery, you can be supported with a care plan.
Education
You will be invited to attend structured education group sessions. They are sessions for newly diagnosed children and their families as well as days for children and young people at specific times like moving to high school or leaving home/going to University.
Immunisations
It is important that all children and young people with diabetes receive their routine immunisations. It is also recommended that in all children and young people on treatment for diabetes have an additional immunisation against pneumococcal infection after the age of 2 years and annual influenza immunisation after the age of 6 months as well.
Transition to young adult services
As you get older (age 12-13 years old) your team will start to talk to you about transition and then at age 16+ you will start to attend transition clinics at the diabetes centre where you will meet other members of the team such as our youth workers who can have different conversations with you around alcohol/driving/university/sexual health etc. We will support you to become more independent with your diabetes.
When you turn 18 years old, you will meet the young adult colleagues with your teams support which will hopefully ensure you have a smooth transfer from the children to the adult services.
E5: Support groups for parents and children
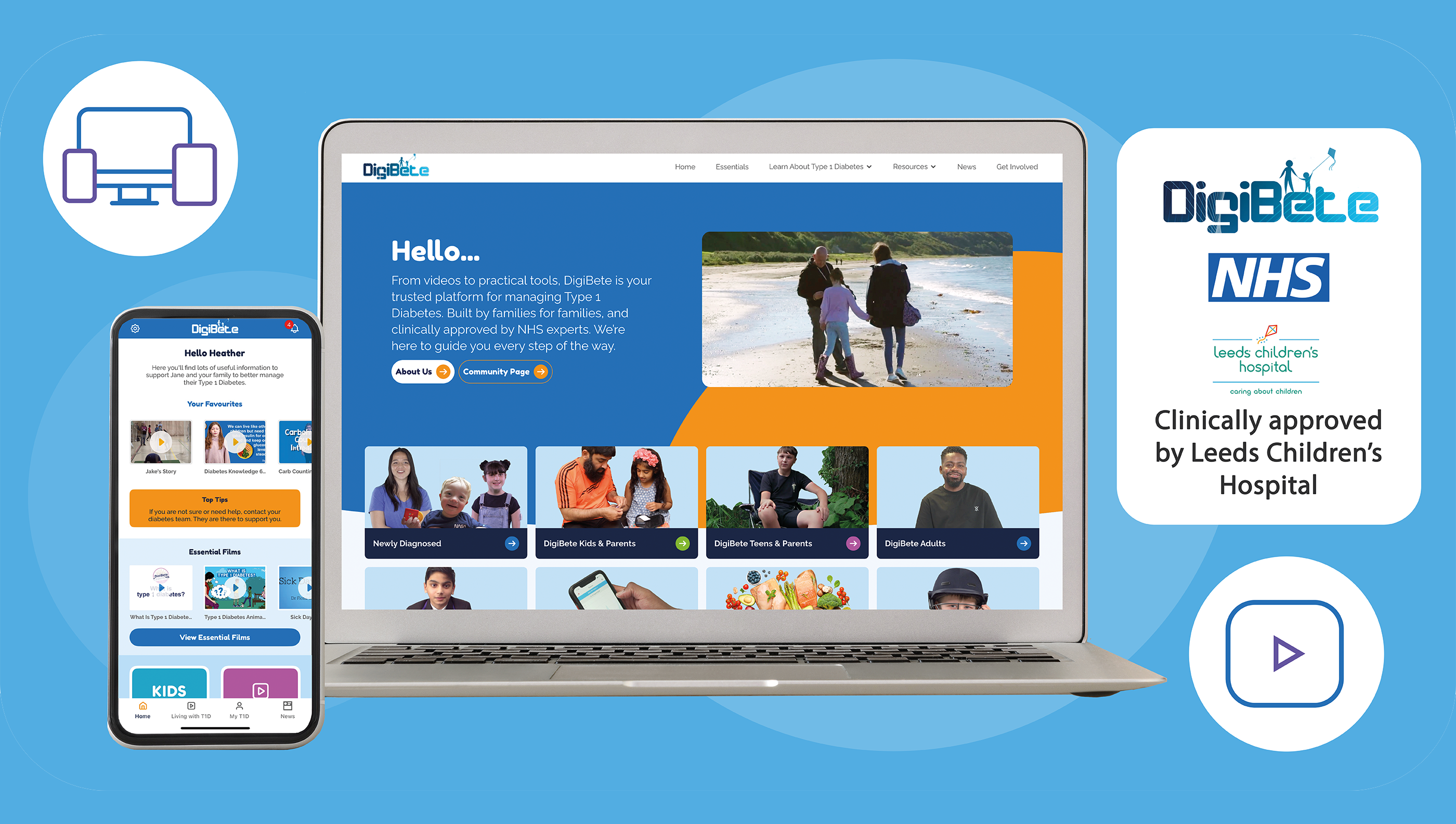
DigiBete
DigiBete is a video platform and App created in partnership with the Diabetes Team at Leeds Children’s Hospital for use by families nationally. The videos are designed to help people and families self manage their Type 1 Diabetes. The DigiBete App is available in England, Wales, Scotland, Ireland and Northern Ireland. Speak to your clinic to get a clinic code. The DigiBete App also complements the information in this workbook.
Breakthrough T1D
Breakthrough T1D is a charitable organisation that funds research into diabetes. They are committed to fundraising and increasing the awareness about the condition and provide information and resources such as the “Talking T1” toolkit and schools training for raising awareness.

Diabetes UK:
Diabetes UK is a charity helping people living with diabetes. It is free for children and families to join for the first year. They provide support and information for people with diabetes, their families and professionals. Diabetes UK organise link weekends for children and families and provide holidays for children of different ages. They have a care line and online information on their website.

E6: If you are over the age of 16
We want you to feel that you can talk to your diabetes team if you smoke, are sexually active, drink alcohol or take drugs. They can offer support and guidance specific to your diabetes and refer you to other agencies if you feel like any of these things are becoming a problem in your life. There are youth workers within the diabetes team who can offer support about life beyond diabetes – education, training, confidence, substance use, social events.
E7: When to contact the team
Your diabetes team is there to help. Please email or contact your nurse if you are not sure what to do next. There is never a daft question!
Some ideas about when to contact your team:
Hypoglycaemia:
- Following a severe hypo.
- If there are more hypos than usual or they occur regularly with exercise.
- If there is impaired hypo awareness or night time hypos.
- Always contact your team if you have any worries or questions.
High glucose levels:
- If there is a trend over a few days with your glucose levels rising into double figures.
- If weekly average glucose levels are rising above 9.0mmol/l.
Variable swinging glucose:
- If glucose levels are swinging and you are uncertain what to do.
Information and conversations shared with the team are confidential, unless it is felt that the individual is putting themselves or someone else at serious risk.