LWD - Chapter B
Practical Skills
B1: Glucose & Ketone meters
Blood glucose and ketone meters help you to check your blood glucose and ketone levels from a finger prick blood sample; they are essential tools to help with your diabetes management. They provide key information to help decisions on how much insulin to give or if you need extra carbohydrates, or to help manage illness and exercise. Your diabetes team will show you how to perform a blood glucose and a ketone check using a meter and a fingerpicker.

How To Check Blood Glucose Levels
How To Check Blood Glucose Levels
Meter tips:
- Make sure you have a working meter as a back up to check blood glucose and blood ketones.
- If your meter stops working, contact the company to request a replacement.
- For your meter to keep accurate results it is important to use it properly and keep it clean. You will also be shown how to test your meter with control solution.
- Replace your meter battery when indicated.
- Glucose and Ketone strips are available on prescription via your GP.
B2: Blood Glucose checking
Procedure for checking / supervising blood glucose check.
Equipment needed: Meter, strips, finger-pricking device, lancet, sharps bin and cotton wool or tissue.
- Ensure hands are washed and dry them thoroughly. (If hands are cold, run them under warm water or shake them to warm them up).
- Insert new lancet or advance the fastclix lancet as taught.
- Insert strip into meter, this will also turn the meter on.
- Prick the side of the finger (it is less painful than the finger tips) avoid the thumb and forefinger.
- Wipe away the first drop of blood with cotton wool or tissue.
- Squeeze a small drop of blood by milking the finger from the base to the tip.
- Hold the strip to the blood and allow the strip to suck up the blood. The meter will beep or the display will start counting down when enough blood is received.
- After a few seconds the blood glucose level should appear on the screen.
- Dispose of lancet and test strip as taught.
- Record blood glucose result.
When to check:
- Before all main meals (breakfast, lunch and tea) - this allows you to correct your blood glucose by adjusting your dose if you are too high or too low.
- Bedtime - to make sure you are not too high or low before bed.
- If you are unwell - this is essential. You may need to check every 2 hours and give extra insulin if blood glucose is high to avoid ketones and DKA.
- Before, during and post exercise or following alcohol ingestion.
- If suspected hypoglycaemia, check to confirm. If unable to check with a meter quickly treat first, then check.
B3: Giving an insulin injection with a pen device
Giving injections to your child may seem worrying at first, because it is a new skill but also because it can feel at odds with your usual role in protecting your child. These feelings are normal and some people find it useful to remind themselves how much better they are making their child feel by giving them the insulin which their body needs.
Remember you are not alone. A Diabetes Nurse or a member of the ward team will support you until you feel able to manage without their help. CYP also find it helpful, to be involved in administering injections in an age appropriate and supported way. Opportunity to practice the skill on a soft toy with the nurse or play specialist initially and then with parents/carers helps to build trust and confidence and increase cooperation and engagement.
Observing the nurse perform the first injection will enable you to see the correct technique, sites used and also how to support your child during the procedure.

Pen devices
Pen devices are available in full and half unit increments, and can be labelled or assigned according to colour eg Red (which we recommend using for Rapid acting insulin).
Smart/connected pens have a memory function to record the dose and time. Further information on the Novopens with step-by-step instructions on giving an injection and how to replace an empty cartridge are available here. Spare and replacement pens are available via GP prescription.
Pen Needles
Pen needles are only used once. The 4 mm pen needle is the smallest available and is recommended for all Children and young people. However, if the child is unable to do their own injection at school, staff will use a safety needle (5mm) to reduce the risk of a needlestick injury. These needles are covered and so can be helpful if the CYP feels anxious when they see the pen needle.

How to give an Injection of Insulin using Safety Needles
How to give an injection of insulin using safety needles
B4: Injection technique, timing, site care and rotation
Injection Technique
If your child needs an injection to be administered for them by a member of staff (school, hospital, carer, then a safety needle (such as the BD Autoshield 5mm) is required to prevent needlestick injuries.
How to give an injection with a pen device:
- Remove the pen cap.
- Attach a new pen needle.
- Prime the needle with 2 units of insulin, holding the pen with needle upright.
- Once a drop of insulin has been seen, the pen is ready to use. If a drop of insulin has not been seen - repeat the procedure.
- Dial the number of units of insulin calculated for food bolus +/or correction bolus.
- Choose the injection site and lift a wide skin fold. This helps to hold the skin steady and avoids injecting into the muscle. A lifted skin fold is recommended for all ages but especially 2-6year olds.

- Inject the pen device needle at 90 degrees and press the plunger as far as it will go. The dial will reset back to zero to indicate that the dose has been administered.
- Count to 10 before removing the pen device to reduce insulin leakage.
- Following the injection, remove the pen needle from the pen using the outer cover (do not try to replace the inner needle cover) and discard carefully in the sharp’s container.
- Replace the pen cap on the pen device.
- Always remove the needle after every injection to minimise the risk of accidental injection and prevent reuse of a blunted needle which will be more painful and cause trauma to the skin.
- Remember that short/rapid acting bolus insulin should be injected into a different site to long-acting basal insulin.

How To Give An Injection Of Insulin
How To Give An Injection Of Insulin

Sharps bins
Use a sharps bin to safely dispose of pen needles. These can be obtained from your GP but usually have to be collected by the council when full.
Insulin Timing
Short/Rapid acting insulin such as Novorapid is injected 15 minutes before food and is also used to correct high glucose levels. Long acting basal or background insulin is given once or twice a day at a similar time and is not related to food intake.
Check that the insulin you are to use has not passed its expiry date. Once insulin is in use, it lasts for four weeks and may be stored at room temperature. Unopened insulin must be stored in the fridge.
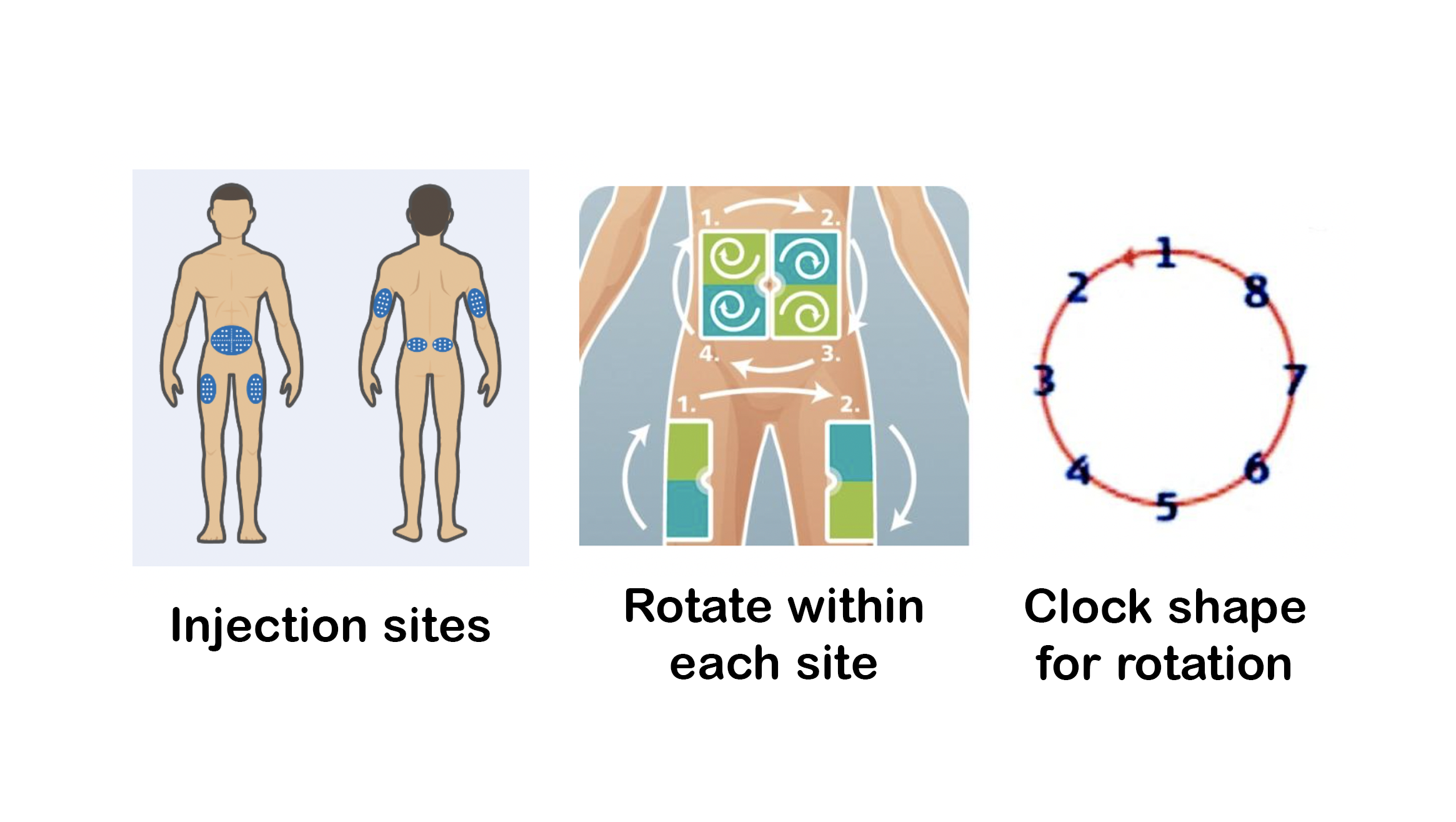
Injection site selection
The preferred site is the top of the buttocks. This area has the most subcutaneous (fatty) tissue which means insulin is less likely to be injected into the muscle. Injecting into the muscle can be more painful and insulin is absorbed quicker and is less unpredictable.
If your child is about to do some activity or exercise such as running or football, insulin injected into the legs will be absorbed very quickly and as the legs have the least subcutaneous fat they are the least favoured site.
There are several rotation patterns suggested (see images below) that help to prevent excessive use of one injection site and ensure optimal absorption of insulin, rather than unpredictable swings from high to low, whilst also reducing the risk of lipohypertophy or fatty lumps.
Rotating fully within one site is the best way to achieve this. Please ask the diabetes team for further advice and support on regularly checking sites for Lipos as they can be tricky to see or feel initially.
B5: Guide to insulin regimes
The two most common types of insulin regimes used are Multiple Daily Injections (MDI) and Insulin Pump therapy (IPT), also known as continuous subcutaneous insulin infusion or CSII.
Both of these involve a basal and bolus insulin being delivered and so are sometimes referred to as “Basal bolus regimes”.
Multiple Daily Injections (MDI)
MDI involves two different types of insulin - a fast acting insulin given as a bolus with each meal or snack and a long acting basal insulin given once or twice a day.
Long acting insulin (Basal)
Long acting insulins are given once or twice daily to provide a low level of background insulin (Basal). This long acting insulin provides a steady release to keep the blood glucose level stable throughout the day and night. Long acting insulin has a slower onset time and lasts much longer than the fast acting bolus insulin. It lasts 20 - 24 hours.
The long acting insulin dose may be split and given morning and evening. Where possible the long acting insulin should be given at a similar time each day.
The long acting insulin is required even when not eating or drinking. It is not fast enough to be used for food or corrections.

Fast/Rapid acting insulin (Bolus)
Fast acting insulin is given for the food to be eaten and when needed to correct a high blood glucose (BG) level. Fast acting insulins such as Novorapid are absorbed more quickly than basal insulin and lasts for 3-5 hours. They are designed to be given before food/drink containing carbohydrate (CHO) to prevent a high blood glucose level or correct back into the target range (4-8mmols/L).
The insulin to carbohydrate ratio (ICR) is the calculation used to work out how much insulin to give before each mealtime. Your diabetes team will guide you re what insulin to carbohydrate ratios to use. It is not uncommon to use different insulin to carbohydrate ratios at each meal. Fast acting insulin works best if given 15-30 minutes before food.
The Insulin Sensitivity Factor (ISF) or Correction dose is the amount of insulin required to bring the BG level back into the target range (4-8mmol/L) e.g. if 1unit lowers the BG level by 5 mmol/L, this will be written as 1:5.

B6: Diabetes Technologies
There are different diabetes technologies available to support diabetes care. These include continuous glucose monitoring, insulin pump therapy and automated insulin delivery systems (AIDs).
Continuous Glucose Monitors
Continuous Glucose Monitoring (CGM) can be used with insulin pump therapy or injection therapy and can reduce the variability of glucose levels, which will help to achieve the time in tight range target (50% of glucose readings between 3.9-8mmol/L). There are a couple of different types available; the diabetes team will decide initially on which sensor will be most suitable.
CGMs work by measuring the fluid underneath the skin (rather than blood) and it shows a sensor glucose (SG) reading every 5 minutes with an arrow showing the direction of change. The sensor readings lag approximately 3-5 minutes behind BG readings because of the way they measure, so it is normal to get a different BG and SG reading, but they should not have a greater difference than 3mmol/L.


Insulin Pump Therapy
Insulin Pump Therapy is another way to deliver insulin; fast acting insulin e.g. Novorapid is delivered continuously under the skin and can be boosted to match meals and give corrections. Its benefits include providing more flexibility, improving time in range and minimising glucose variability.
There are a few different pump options available; the diabetes team will provide guidance on which would be most appropriate depending on lifestyle/age/insulin requirement.
A couple of helpful key words to know are:
- Basal insulin is the background insulin in the pump. It replaces the long acting or background insulin injection.
- Bolus insulin is the insulin that is given for food or corrections.
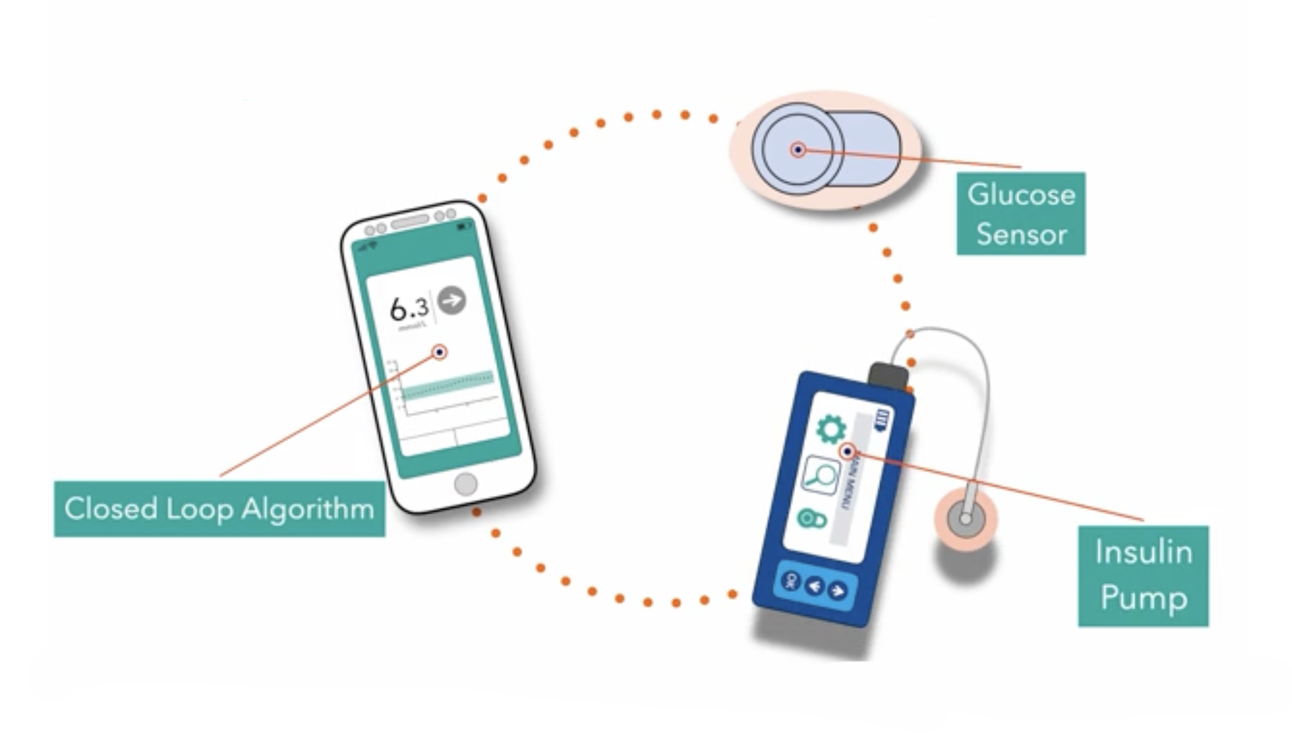
Automated insulin delivery (Closed Loop) systems
Automated insulin delivery (Closed loop) systems consist of three parts:
• Insulin Pump.
• Continuous Glucose Monitor.
• Algorithm.
When the glucose is predicted to go lower than the set target, the pump will automatically suspend the insulin delivery and when the glucose is predicted to go higher than the target, the pump will give more insulin in the background. This system is trying to mimic the function of a working pancreas. It means the pump will help out in the background but it still needs to be told when food is being eaten or activity carried out.
The diabetes team will offer you insulin pump therapy within the first few weeks of your diagnosis. You can look at the different pumps available so we can all decide together which would be most suitable. A smartphone is usually required for CGM and AIDs so the diabetes team will also talk about access and support to enable this. Some pumps have a 4-year contract which will be explained to you if you choose one. Please expect more clinic visits before after a pump start so we can give you the right amount of support and guidance.
Click on the image to learn more about diabetes technology on the technology page.
B7: Monitoring and taking care of your diabetes
Your body works best if your blood glucose levels are not too high and not too low. People who do not have diabetes have blood glucose levels that stay between 3.5 and 7 mmol/L. If you have diabetes, the goal is to keep your blood glucose levels between 3.9 and 8 mmol/L before meals and on waking, and between 5 and 9 mmol/l approximately 2 hours after meals most of the time. Careful balancing of your insulin doses, diet and exercise will help towards achieving this.
Measuring your blood glucose is the only way of knowing exactly what your levels are. If you go by how you feel, you will only know when you are very low or very high. Without any reading, your diabetes team will find it more difficult to advise you, so it is important to either bring your meter to clinic or have your sensor data linked to the clinic.
Daily blood glucose monitoring
This can be done by either monitoring your sensor glucose (SG) readings or by doing regular BG finger prick checks, with the equipment we will give you (see blood glucose checking). It can be done at home, school, out with friends and on holiday!
It is recommended that you check your glucose levels at least before each meal, before bed and when you feel low (hypo) or unwell. If your glucose level is high (greater than 8 mmol/L) it is important to check that it has come back to normal within 4 hours. Extra consideration needs to be taken for AIDs which you will be taught at your pump start.
The children who obtain optimal glucose levels check their BG on average 5 to 7 times each day or have a sensor usage time of over 90% (the CGM is on and working over 90% of the time) and achieve 50% of their results in the tight target range.
Extra checks may be needed at other times such as during illness, following a hypo, stressful periods such as exam time or during a growth spurt.
Patterns and trends of blood glucose levels that are too high or too low are more easily identified with regular monitoring.
If blood glucose levels are significantly high (14mmol/L or more), check for blood ketones.
If blood ketones are above 0.6mmol/L and rising, immediate action must be taken because you are in danger of becoming seriously ill very quickly. (See sick day rules).
The importance of measuring and monitoring blood glucose levels
The blood glucose or sensor glucose number tells you the glucose level at that moment (remember SG has a 5-10 min lag time).
Recommended blood glucose target ranges for children with diabetes are:-
- On waking: 4 to 8 mmol/L.
- Before meals at other times of day: 4 to 8 mmol/L.
- After meals: 5 to 9 mmol/L.
- Before driving: At least 5mmol/L.
The glucose result helps you to plan what action you need to take to manage your diabetes on a day to day basis but also helps you to spot patterns and trends. E.g. if the glucose level is high e.g. 8mmols/L or more before a meal then additional insulin is recommended. This is called a CORRECTION DOSE.
This extra insulin is added to the food bolus insulin which has been calculated from carbohydrate counting. Within 2-4 hours or by the next meal the blood glucose level should then return into the target range. You will be informed of your correction dose ratio by the diabetes team. The correction dose ratio will change over time as you grow.
Looking for patterns and trends of rising or low blood glucose levels, and looking for reasons for these, will give you clues as to the changes required to get back to your target level. Before changing insulin doses you need to consider other things, such as injection sites, rotation, exercise and food (see insulin adjustments and problem solving).
B8: HbA1c or Glycated Haemoglobin
HbA1c or glycated haemoglobin is an indication as to what your blood glucose levels have been on average over the last 6-12 weeks.
What does it measure?
Haemoglobin is present in red blood cells (the Hb of HbA1c) - this is what makes your blood red. Glucose sticks to red cells and the more glucose there is around in the blood, the more red blood cells have glucose attached. The average lifespan of a red blood cell is 120 days and therefore if we measure how many red blood cells have glucose attached to them, it gives us a guide as to the glucose levels in your blood over the last 120 days (3 months).
What it does not measure?
This can be the confusing bit. It is not a measure of blood glucose as you would get if you are doing a finger prick and testing your blood with a meter. It does not measure sudden changes in your glucose levels and it will not reflect a single day or week when glucose levels have been higher or lower than target.
Why are HbA1c and average glucose levels important?
Small blood vessels run throughout the body and get damaged by persistently high blood glucose levels which lead to long-term complications of diabetes, such as kidney and eye problems. A HbA1c target level of 48 mmol/mol (6.5%) or lower is ideal to minimise the risk of long-term complications. This requires hard work to achieve but is worth it. It is important to note if HbA1c levels are above the ideal target of 48mmol/mol or less, that any reduction in HbA1c level reduces the risk of long-term complications.
Children and young people with type 1 diabetes and their family members will be supported to safely achieve and maintain their individual agreed HbA1c target level.
How often is it measured?
The aim is to measure HbA1c at every clinic visit, at least every 3 months. If it is above 69 mmol/mol (8.5%), more frequent appointments will be arranged to provide you with additional support.
After the diagnosis of Type 1 diabetes, the first two years are especially important. Research has shown that achieving target glucose levels and a HbA1c less than 48mmol/mol within the first 12-24 months is protective of future health. You will be supported to reach this glucose target within 3-6 months of diagnosis and maintain for as long as possible, by proactive management, using technology and providing practical and emotional support to you and your family. The “First Year of Care Pathway” is to help achieve a good start with diabetes – this will be discussed with you in clinic.
B9: Average blood/sensor glucose levels and meter uploads
At home
The HbA1c level effectively represents average glucose levels over a period of 6-12 weeks. A way of monitoring how you are doing between clinic visits is by looking at your average blood glucose levels over 1-2 weeks and you can do this on your glucose sensor. The relationship between an average glucose level and HbA1c is shown in this chart below.
HbA1c (mmol/mol). - Average glucose(mmol/L)
- 20-42. 3.8-7
- <50 <8.1
- 50-60 8.1-9.5
- 61-70 9.6-11.1
- 71-80 11.2-12.5
- 81-100 12.6-15.4
- >100 >15.4
To meet the national target for an HbA1c of 48mmol/mol or less, we would suggest that you aim for a weekly average blood glucose level of 8mmol/L or less. It is also possible to look at the percentage of results within target, an example of which as shown below.
The aim is to try and have at least 70% of the results between 3.9 and 10mmol/L.
- 1% - Very High - >13.9mmol/L
- 7% - High - 10.1-13.9mmol/L
- 88% - Target Range - 3.9-10mmol/L
- 3% - Low - 3-3.8mmol/L
- 1% - Very Low - <3mmol/L
% Time CGM Active 96.6% (13.5days)
- GMI: 6.4% (46.1mmol/mol)
- Average: 7.1mmol/L
- SD: 2.1mmol/L
- CV: 29.3%
- Median: 7mmol/L
- Highest: 16.8mmol/L
- Lowest: 2.6mmol/L
Ideally >50% of glucose levels will be between 3.9 and 8 mmol/L.
- 1% - Very High - >13.9mmol/L
- 31% - High - 7.9-13.9mmol/L
- 64% - Target Range - 3.9-7.8mmol/L
- 3% - Low - 3-3.8mmol/L
- 1% - Very Low - <3mmol/L
% Time CGM Active 96.6% (13.5days)
- GMI: 6.4% (46.1mmol/mol)
- Average: 7.1mmol/L
- SD: 2.1mmol/L
- CV: 29.3%
- Median: 7mmol/L
- Highest: 16.8mmol/L
- Lowest: 2.6mmol/L
If your glucose average is regularly above 8mmol/L or if you are having hypos more than 4% of the time, please contact your diabetes team so that they can help to see if any changes need to be made to insulin doses or timing.
In Clinic
When you attend your diabetes outpatient clinic your meter and/or sensor data will be reviewed and discussed with you at your consultation. The same will apply to your insulin pens or pump. It is therefore essential that all your equipment is brought to clinic and that the time and date is correct on your devices.
The Glooko system is used in many hospitals and enables the uploading of several different
diabetes devices and the results displayed on tables and graphs.
Most clinics targets now:
- Average BG or SG (over 14 days) - 8mmol/L
- Standard deviation (variability) - <3mmol/L
- Time in range (4-10mmol) - 70%
- Time in tight range (3.9-8mmol/L) - 50%
B10: Uploading and sharing data
The data collected on the technology you have been provided with is to aid in caring for your diabetes. This can be viewed by you and your family/carers and shared with your diabetes team. It allows a visual representation of your glucose levels and insulin doses over a set time e.g. 2 weeks. Changes can be made from this data to optimise your diabetes management.
Glooko allows easy uploading of information from most, but not all, glucose meters, insulin pumps, CGM and mobile apps. For technology that does not upload to Glooko, other companies have different platforms to download their devices.
The diabetes team will support you to ensure you have access to all your data.
