LWD - Chapter A
Introduction and Explanation of Type 1 Diabetes and Treatment
A: Explanation of Type 1 Diabetes and Treatment
A1: What is Type 1 Diabetes?
The most common type of diabetes in childhood in the UK is Type 1 Diabetes. It affects over 30,000 children in the UK. Type 1 diabetes should not be confused with Type 2 Diabetes, which is usually diagnosed in adults and is associated with lifestyle factors.
In Type 1 diabetes your body loses the ability to regulate the level of glucose (sugar) in your blood due to a failure to make insulin. Glucose levels in the blood are usually controlled very accurately between about 3.9 to 7mmol/l.
Insulin is one of the key chemicals or hormones that regulate the body's blood glucose levels. Insulin is made in cells (islet cells) found in the pancreas, an organ found behind the stomach. Type 1 diabetes occurs because the body’s own immune system attacks these cells and the body is unable to make enough insulin. Getting glucose levels in range early will help preserve some islets cells for a time, making it easier to maintain normal blood glucose levels.
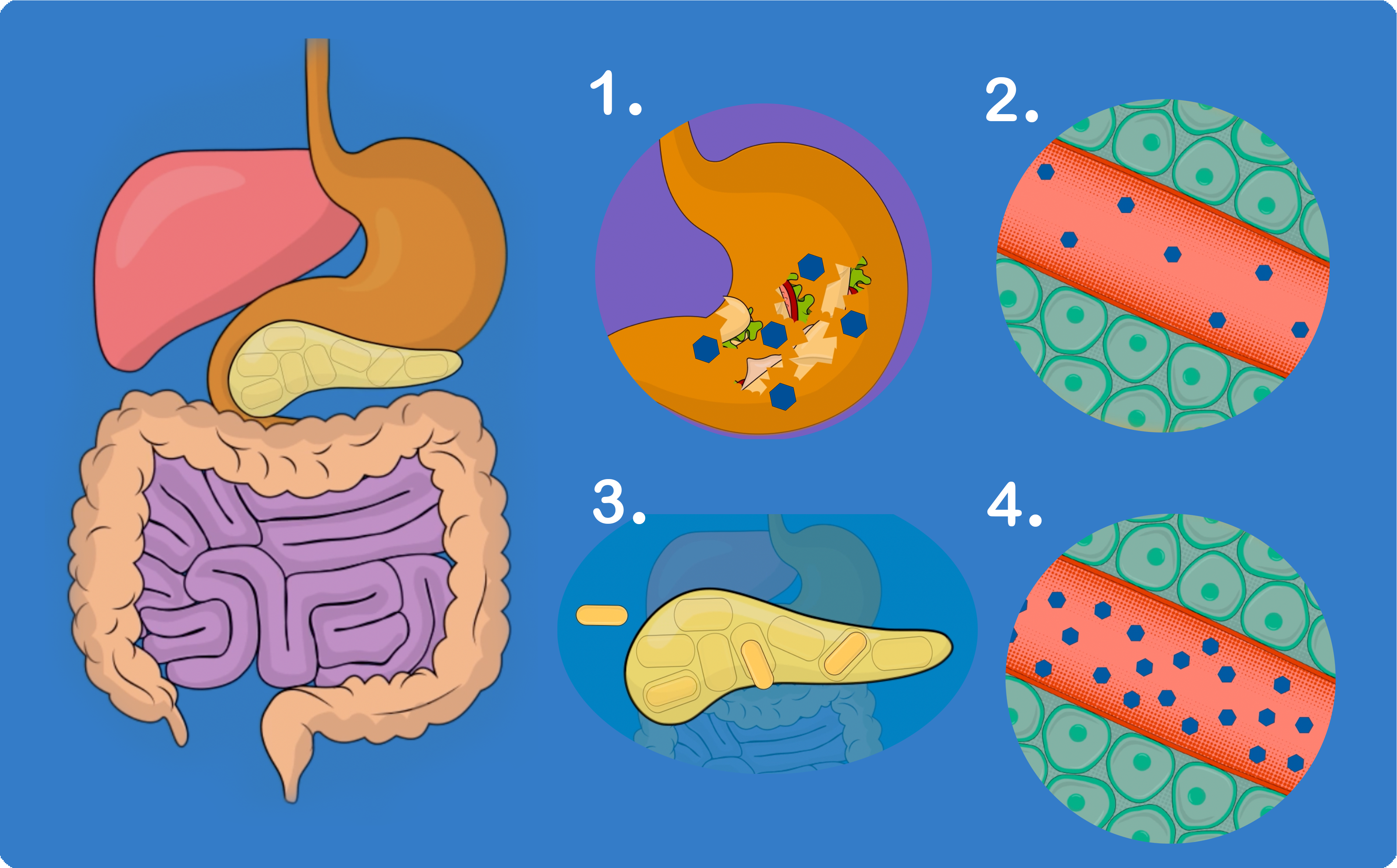
- The stomach changes food into glucose.
- Glucose enters the bloodstream.
- The pancreas makes little or no insulin - Little or no insulin enters the bloodstream.
- Glucose builds up in the bloodstream.
Key message: Type 1 diabetes is due to the body’s inability to make sufficient insulin and control glucose levels.
Type 1 Diabetes Animated Explainer
An animated explainer video introducing Type 1 Diabetes
What is Type 1 Diabetes
How Insulin Works
We know that insulin is the vital 'messenger' which helps convert the food we eat into energy, by allowing glucose to pass from the blood to all the cells in the body. The sweet and starchy food we eat and drink, (carbohydrates) are broken down into glucose (sugar) in the stomach and intestines; the glucose then passes into the blood stream. Insulin allows the glucose to be used as fuel for all our daily activities, even for sleeping, to ensure adequate growth and to repair cells when damaged. Insulin also transfers any extra glucose in the blood stream to muscles, fat cells and the liver to be stored until it is needed for energy.
Extra energy is required for exercise and during emergencies, e.g. when we are unwell. The body uses up the energy stored in our muscles and liver for these occasions. If the energy stores are empty due to a failure of glucose to cross from the blood to tissues, the body uses fat for energy. This explains why tiredness and loss of weight are common signs of diabetes.
Without insulin, the glucose from food and drink in the form of carbohydrates stays in the blood stream causing the blood glucose level to rise; some is filtered through the kidneys and then passed out of the body in the urine, taking water from the body along with it. This explains why many children drink (polydipsia) and wee a lot (polyuria), sometimes day and night before diagnosis or if their diabetes is out of range. High blood glucose levels can also increase the risk of infections.
The amount of insulin being produced by your pancreas would have been slowing down for a considerable time (weeks-months) so sometimes the onset of the symptoms may have been gradual and can often go unrecognised for some time. Occasionally the presentation can be dramatic with severe dehydration, rapid breathing and profound vomiting. This is diabetic ketoacidosis (DKA) and requires urgent and careful treatment and is potentially life threatening.
How We Can Treat Diabetes
The body now needs help to process the glucose that is taken as carbohydrates in food and drink; otherwise you will continue to feel unwell and eventually develop diabetic ketoacidosis. We can do this by giving you insulin that your body is not able to make itself. Insulin has to be delivered to the area under the skin and it is therefore given by an injection or tiny cannula (if using an insulin pump).
Insulin has to be given in a dose which matches the carbohydrate content of the food and drink we eat at meals and snacks; this is called carbohydrate counting. The dose of insulin given with food and drink is called “bolus insulin”. Your body, even when not eating, always has a low level of insulin in the blood stream. This is important to deal with glucose released from the liver and muscles and is called “basal insulin”, and is given once or twice every day and is not related to food.
Key message: The children’s diabetes team will be able to teach you how to care for
diabetes and offer you on going help and support.
What is Type 2 Diabetes?
It is possible to be diagnosed with type 2 diabetes as a young person even though it is often considered to be a disease in older people. It is just as serious as type 1 diabetes but will require different treatments and education sessions. With type 2 diabetes the body does make insulin but the insulin does not work well enough to keep the blood glucose in the normal range.
Other types of Diabetes
There are other types of diabetes, including steroid induced diabetes, cystic fibrosis related diabetes, some rare genetic syndromes and types of monogenic diabetes.
Monogenic diabetes is diabetes caused by a change in a single gene. It runs in families and is passed on directly from a parent to a child so does not ‘skip a generation’. It includes Neonatal Diabetes and types of MODY (Maturity Onset Diabetes of the Young). This can be caused by a change in quite a few different genes and the treatment needed will depend on which gene is affected. Further information can be found on the website www.diabetesgenes.org. or you can discuss the local Genetic Diabetes Nurse.
A2: Diabetes supplies and medication
You will need a variety of equipment and medication on repeat prescription to look after your child’s diabetes at home. Not all the equipment will be needed every day, but may be needed for illness management, so it is important that it is always available and in date.
Equipment and medication required at home:

- Insulin - Bolus Insulin and Basal Insulin 1 box of 5 cartridges or 1 box of 5 disposable pens or an insulin vial.
- 2 Insulin pen(s) - with half unit increments.
- Insulin pen needles - 1 box of 100 needles 4mm.
- Safety Pen needles - For school or 3rd party use (4 or 5mm).
- Finger-pricking lancets.
- Blood glucose strips.
- Blood ketone strips.
- Blood Glucose/Ketone meter.
- Lift glucose tablets or Lift glucose drinks.
- Glucagon kit.
- Sharps bin.
The above items are available on repeat prescription from your GP. You will be given a small supply when you leave hospital but will need to set up a repeat prescription.
Additional supplies will be needed if your child is discharged home on an insulin pump. These will come directly from the insulin pump company. Your diabetes nurse will set this up for you.
You will also be given a finger-pricking device, a meter to check blood glucose and ketones. These items are not available on prescription. Please complete and return the warranty card which comes with your meter. This will enable you to contact the company directly via the customer care line to order control solution or discuss any problems.
Storage and use
Insulin
- Insulin in use or if carried as a spare should be kept at room temperature, do not refrigerate. Store below 30°C. Use within one month.
- Store unused insulin in a refrigerator. Keep away from the cooling element. Do not freeze. Insulin will last until the expiry date when stored this way.
- Keep cartridges not in use in the outer carton in order to protect from light.
- Keep the cap on insulin pens in order to protect from light.
- Protect from excessive heat and light.
Pen needles and lancets
- A new pen needle or lancet should be used for each blood check or injection.
- Must be disposed of into a sharps bin.
- Store at room temperature.
- Remove pen needle after injection and store pen without a needle attached in order to prevent air from entering the cartridge and reduce the risk of injury.
Blood glucose and ketone strips
- Store strips at room temperature.
- Keep strips within the closed container or sealed in foil wrapper.
- Do not use strips if they have been damaged in any way or are out of date.
Glucagon Injection Kit
- Store either in a refrigerator (2°C to 8°C), or out of a refrigerator below 25°C for up to 18 months before the expiry date.
- Store in original package to protect from light.
- Do not freeze, to prevent damage to the product.
- Do not use after the expiry date stated on the label. The expiry date refers to the last date of that month. (You could use the expired Glucagon to practice the technique of preparing and mixing the solution)
- Do not use if the solution, in rare cases, looks like a gel or if any of the powder has not dissolved properly
- Smaller children will not require the full amount, your diabetes nurse will advise about this.
GlucoGel/Dextrogel
- Keep GlucoGel/Dextrogel at room temperature.
- If GlucoGel/Dextrogel is put in the fridge, the composition of the gel will not change but it will become thicker and harder to administer. If the gel has been kept in the fridge, allow it to reach room temperature again before using.
Medicines should not be disposed of via the wastewater pipes or via household waste. Ask your pharmacist how to dispose of medicines which are no longer required.